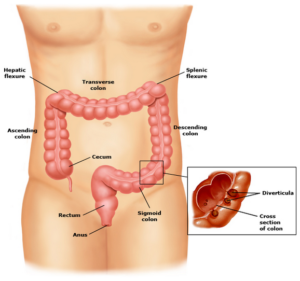
Diverticulitis is a condition related to diet that affects nearly half the Americans older than age 60, which have small, bulging pouches (diverticula) in their digestive tracts, a condition known as diverticulosis. Although diverticula can form anywhere, including in your esophagus, stomach and small intestine, most occur in your large intestine — especially on the left side of the colon just above the rectum. Because these pouches seldom cause any problems, you may never know you have them.
Sometimes, however, one or more pouches in the colon may become inflamed or infected, causing severe abdominal pain, fever, nausea and a marked change in your bowel habits. When diverticula become infected, the condition is called diverticulitis. Mild cases of diverticulitis can be treated with rest, changes in your diet and antibiotics. But serious cases may require surgery to remove the diseased portion of your colon. Occasionally, you may develop complications that require emergency surgery.
Fortunately, only 15 percent to 20 percent of people with diverticulosis ever develop diverticulitis. Best of all, you can help prevent both types of diverticular disease by including more high-fiber foods in your diet.
 Signs and Symptoms of Diverticulitis
Signs and Symptoms of Diverticulitis
Diverticula can feel like appendicitis, except you’ll generally have pain in the lower-left side of your abdomen, instead of the lower-right side. The pain is usually severe and comes on suddenly, but sometimes you may have mild pain that becomes worse over several days and fluctuates in intensity. You may also have abdominal tenderness, fever, nausea, and constipation or diarrhea.
Less common signs and symptoms of diverticulitis may include:
- Vomiting
- Bloating
- Bleeding from your rectum
- Frequent urination
- Difficulty or pain while urinating
Causes of Diverticulitis
Diverticula usually develop when naturally weak places in your colon give way under pressure. This causes marble-sized pouches to protrude through the colon wall. Pouches are most common in your sigmoid and descending colon — the lower portions of your large intestine just above your rectum — and often occur as a result of straining during bowel movements over a number of years. The pouches are small at first but become larger with time.
Sometimes a bit of stool may become lodged in one of the pouches, leading to infection. A small tear or perforation can also develop in an infected pouch, which in turn can cause an infection within your abdomen (peritonitis). If the infection is limited to an area around the wall of your colon where the diverticula are inflamed, you may develop a localized collection of pus known as an abscess.
Prevention of Diverticulitis
The following measures can help prevent or slow the progression of diverticular disease:
- High-fiber foods, such as fresh fruits and vegetables and whole grains, soften waste material and help it pass more quickly through your colon. This reduces pressure inside your digestive tract. Aim for 25 to 30 grams of fiber each day. Try to substitute fruits, vegetables and grain products for foods high in fat. Be sure to add fiber gradually to avoid bloating, abdominal discomfort and gas. If you have a hard time consuming 25 to 30 grams of fiber every day, consider using a fiber supplement such as psyllium (Metamucil, Fiberall) or methylcellulose (Citrucel).
- Drinking plenty of fluids. Fiber works by absorbing water and increasing the soft, bulky waste in your colon. But if you don’t drink enough liquid to replace what’s absorbed, fiber can be constipating. Try to drink at least eight 8-ounce glasses of water or other beverages that don’t contain caffeine or alcohol every day.
- Responding to bowel urges. When you need to use the bathroom, don’t delay. Delaying bowel movements leads to harder stools that require more force to pass and increased pressure within your colon.
- Exercise promotes normal bowel function and reduces pressure inside your colon. Try to exercise at least 30 minutes on most days.
Treatments
In general, your treatment depends on the severity of your symptoms and whether this is your first attack of diverticulitis. If your symptoms are mild, a liquid or low-fiber diet and antibiotics may be all you need. But if you’re at risk of complications or have recurrent attacks of diverticulitis, you may need more advanced care.
Home care
If your condition calls for home treatment, expect to remain quiet for a few days. You’ll also temporarily need to avoid all whole grains, fruits and vegetables, so your colon can rest and heal. Once your symptoms improve, often in two to four days, you can gradually start increasing the amount of high-fiber foods in your diet.
In addition, your doctor will likely prescribe antibiotics to help kill the bacteria causing your infection. Even if you start feeling better, be sure to finish your entire course of medication. Stopping too soon could cause your infection to come back. It also helps create strains of bacteria that are resistant to antibiotics. If you have moderate or severe pain, your doctor may recommend an over-the-counter pain reliever such as acetaminophen (Tylenol, others) or a prescription pain medication, although these medications tend to be constipating and may aggravate the problem.
Hospitalization
About half the people with diverticula require hospitalization and many need intravenous antibiotics. You’re more likely to be hospitalized if you have vomiting, a fever above 100 F, a high white blood cell count or are at risk of complications such as a bowel obstruction or peritonitis. You’re also likely to need additional care if you are older, have another disease or have a weakened immune system.
Diverticulitis Surgery
If you have recurring diverticulitis, your doctor may recommend surgery to remove the diseased part of your colon. There are two types of surgery:
- Primary bowel resection – This is the standard surgery for people with diverticula. Your surgeon will remove the diseased part of your intestine and then reconnect the healthy segments of your colon (anastomosis). This allows you to have normal bowel movements. Depending on the amount of inflammation, you may have open (traditional) or laparoscopic surgery. In open surgery, your surgeon makes one long incision in your abdomen, while laparoscopic surgery is performed through three or four tiny incisions. You’ll heal faster and recover more quickly with laparoscopic surgery. Unfortunately, it may not be an option if you are very overweight or have extensive inflammation.
- Bowel resection with colostomy – This surgery may be necessary if you have so much inflammation in your colon that it’s not possible to rejoin your colon and rectum. During a colostomy, your surgeon makes an opening (stoma) in your abdominal wall. The unaffected part of your colon is then connected to the stoma, and waste passes through the opening into a bag. A colostomy may be temporary or permanent. Several months later — once the inflammation has healed — your surgeon may be able to perform a second operation to reconnect your colon and rectum.
These links will redirect you to…